myCare Start
Title
Implementation of a new model of care for supporting adherence in people starting a new medication for a long-term condition (myCare Start-I project) – An implementation-effectiveness study
Project Lead
Marie-Paule Schneider Voirol
Sabina De Geest (project co-lead)
INS-Team
Sabina De Geest
Juliane Mielke
External Partner
University of Geneva, Institute of family and child medicine (Prof. Dagmar Haller, Dr. Cédric Lanier)
University of Geneva, Research Institute for Statistics and Information Science (Prof. Stéphane Guerrier)
Patient Partner (Kabeza Kalumiya)
Unisante (Prof. Joachim Marti, Dr. Clemence Perraudin, Giulio Cisco)
University of Basel (Prof. Samuel Alleman, Selina Barbati, Linnéa Simona Walti)
University of Bern (Prof. Alice Panchaud)
University of Bern/pharmaSuisse (Dr. Stephen Jenkinson, Fanny Mulder)
Avedis Donabedian Research Institute (FAD) (Dr. Alexandra L. Dima)
Universitat Autònoma de Barcelona (UAB),
Avaluació de tecnologies sanitàries en atenció primària i salut mental (PRISMA),
Institut de Recerca Sant Joan de Déu (IRSJD),
Consortium “Centro de Investigación Biomédica en Red” Epidemiology and Public Health (CIBERESP)
Location of Data Selection
Switzerland
Duration
2022 bis 2026
Description
Background
In Switzerland, a quarter of the population (2.2 million persons) live with a non-communicable chronic disease, a prevalence that is expected the increase as the population ages. The majority of chronic patients are on long-term medication regimens which requires patient’s active participation in care and responsible self-management, including optimal adherence to medications. However, poor medication adherence upon initiation of long-term treatment is of particular concern and necessitates interprofessional action in primary care (i.e., physicians in collaboration with trained pharmacists and nurses).
One of the best evaluated, evidence-based, interprofessional interventions to reinforce early adherence after medication initiation, is the UK developed patient-centered New Medicines Service (NMS). Effectiveness studies revealed a 10% increase in the number of adherent patients receiving NMS at 10 weeks, with overall reduced costs to the NHS in the long term. Since then, the NMS has been implemented in several European countries (England, Ireland, Scotland, Denmark and Belgium). However, implementation failures limited its effectiveness in real-world settings.
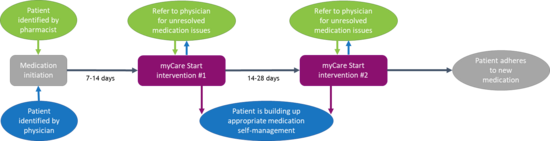
Based on the NMS, myCare Start was introduced by pharmaSuisse into Switzerland. It is the first evidence-based, nation-wide health service, conducted by interprofessional primary care teams to support medication adherence in chronically ill patients starting a new long-term treatment in Switzerland. The service consists of 2x10 minute semi-structured pharmaceutical interventions tailored to the patient’s needs, positioned as partner, during the first 6 weeks after treatment initiation. A feasibility study, confirmed the potential of myCare Start in Switzerland. However, implementation challenges including reach of pharmacies, poorly developed interprofessional collaboration and patient attrition highlight the need for implementation science methods to ensure the successful implementation and maximum impact of myCare Start.
Objectives
To adapt the NMS for Switzerland (myCare Start) and implement and evaluate myCare Start within Switzerland’s community pharmacy-physician network to enhance medication adherence during the initiation of a new chronic treatment.
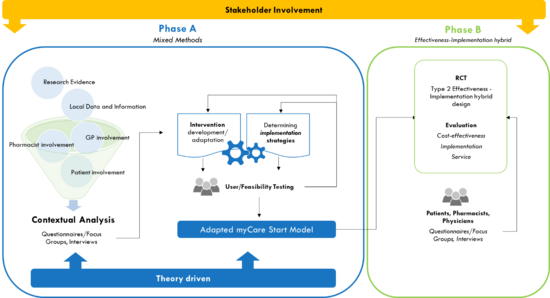
Phase A
- To conduct a contextual analysis of the current Swiss primary care ecosystem as related to pharmacy-physician interprofessional health services for chronic care patients.
- To engage key stakeholders within the Swiss primary care ecosystem to contribute to the creation of a Swiss interprofessional myCare Start service.
- To design a contextually adapted myCare Start for use within Swiss community practice using contextually appropriate implementation strategies.
- To conduct feasibility testing on the contextually adapted intervention and implementation strategies and to develop an implementation research logic model.
Phase B
- To implement e a contextually adapted Swiss myCare Start intervention within Switzerland’s community pharmacy-physician network and evaluate it terms of medication adherence and cost-effectiveness outcomes.
- To evaluate implementation outcomes and the implementation pathway of myCare Start.
Design/Method
MyCare Start is an interprofessional, multicentric, national implementation science project conducted in collaboration with six university partners and across 160 community pharmacy-physician networks in Switzerland. The research project includes two phases focusing on adaptation, implementation (phase A) and evaluation (phase B).
Phase A:
- Using state-of-the art stakeholder involvement methods, a interprofessional stakeholder group will be initiated to provide advice, expertise and direction to build a strong foundation for the myCare Start intervention and ensure its long-term viability. Stakeholders will be engaged throughout the different project phases, including the adaptation, implementation and evaluation of the myCare start intervention, as well as to establish interprofessional collaboration models with physicians, nurses and patients.
- A contextual analysis will be conducted as foundational phase to inform subsequent steps of the myCare Start project. The contextual analysis builds on existing evidence on implementation barriers in real-world from international and Swiss studies. Additional primary data collection by mixed-methods will be conducted to map practice patterns and structural characteristics of pharmacies in Switzerland; (2) to identify unmet needs and relevant contextual factors regarding chronic disease management in pharmacies; (3) Assess innovation climate and openness regarding myCare Start; (4) to understand factors that drive implementation of myCare Start and how they are interconnected.
- Adaptations of myCare start will be co-created with stakeholders to ensure real-world translation. Given the variety of settings where myCare Start will be delivered, core and adaptable implementation components will be defined. Educational and behavioral intervention components will be theory-driven.
- Alongside stakeholders, multi-level, contextually adapted implementation strategies supporting myCare Start implementation in practice will be selected based on the ERIC (Expert Recommendations for Implementing Change) taxonomy.
- A multi-method feasibility study will be conducted in 12-15 pharmacies to pre-test contextually-adapted implementation strategies.
- An implementation research logic model indicating the relationship between inputs (determinants), activities (implementation components and implementation strategies), outputs (implementation mechanisms) and outcomes will be developed.
Phase B:
Using a hybrid type II effectiveness-implementation design (two-arm, multi-center, stepped wedge cluster randomized controlled design), myCare Start will be implemented and tested in 120 pharmacies in Switzerland. Medication adherence as primary outcome will be measured at 10 weeks, 6 and 12 months using the BAASIS® patient-self report and electronic pharmacy refill records. A 12-month cost-utility analysis will be performed from a healthcare system perspective. Guided by the NoMAD tool (Normalization Measure Development questionnaire), implementation outcomes (i.e., reach, adoption, fidelity, acceptability and implementation costs) and the implementation pathway will be assessed using mixed-methods.
Expected Benefit/Relevance
MyCare Start will be the first innovative, interprofessional, integrative care model to support medication adherence in chronically ill patients in Switzerland. Collective efforts to improve patient adherence to long-term therapy may improve patient therapeutic outcomes, safeguard patient safety and alleviate the financial burden on patients and the health system. MyCare Start will not only provide evidence regarding the effectiveness of the intervention, but will also generate much-needed insight into how to implement the intervention in real-world settings, a prerequisite for further scale-up.